X-ray Mammography
To date, X-ray mammography is the “gold standard” for breast screening and diagnosis. During the past two decades, mammography screening has reduced the mortality rate among women with breast cancer considerably, by detecting approximately 85-90% of breast cancers. It is recommended that asymptomatic women above certain age undergo annual breast X-ray mammography.
During the test breast is exposed to an X-ray beam whose transmission is measured. The breast is compressed between an X-ray sensitive screen and a transparent plate to:
- Obtain a uniform thickness
- Reduce the total thickness in order to facilitate operation in the range of lower photon energy levels and higher contrast between tissues, to obtain a clearer image, and
- Reduce overlapping of the different inner breast tissues to increase clarity of the image and better sensitivity.
Regular screening mammography undoubtedly saves lives – it is estimated that for every 1000 women who undergo regular screening mammography, 1.8 lives will be saved. But mammography is not without its risks and costs. It is X-ray based and provides reasonable spatial resolution, allowing for the detection of morphological modifications (i.e., asymmetry, ill-defined boundaries). The procedure is rapid, cost-effective and generally accurate. However, it has several recognized weaknesses:
- False Negatives - According to Medtech Insight, screening mammography produces false negatives in as many as 20% of the cases. Several published investigations have suggested that while mammograms of normal breast tissue miss only 2% of cancerous tumors, mammograms of the most dense breast tissue (i.e., younger women or women with breasts possessing high amounts of radio-dense glandular tissue) suffer from poor interpretation and fail to detect up to 52% of cancers. This is particularly significant since published studies have suggested that women with dense breast tissue, who represent about 40% of the female population in the USA and 90% of Asian population, are also at higher-risk to develop cancer;
- False Positives - Approximately 7% of all mammograms yield false positives and result in needless anxiety, more examinations, and unnecessary biopsies;
- Unable to distinguish between a cyst and a solid mass;
- Unable to characterize a mass (benign vs. malignant);
- It uses ionizing radiation with its potential carcinogenic risks, especially in screening asymptomatic women who may be exposed for at least 25 times before the age of 70;
- Provides 2-D projection of the breast. Therefore two or more projections are needed to precisely detect the lesion.
In many developed countries, the film-screen mammography (FSM) is being gradually replaced by full-field digital mammography (FFDM) which is identical to FSM except for the electronic detector that captures and facilitates display of the X-ray signals on a computer or laser-printed film. Although the resolution of the new FFDM instruments is not higher than the traditional FSM technique, additional data processing may help to find tumor marks with higher accuracy.
For more information, visit: http://en.wikipedia.org/wiki/Mammography
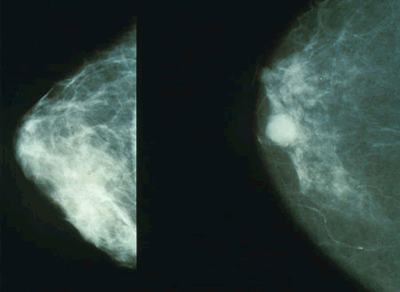
Left: Benign. Right: Malignant


